Immunotherapy Cancer Treatment
Immunotherapy is a broad category of anti-cancer therapies that uses the body’s immune system to fight cancer cells. The immune system — made up largely of the lymph nodes — rids the body of viruses, bacteria or fungi, while white blood cells such as T cells fight infection and cancer.
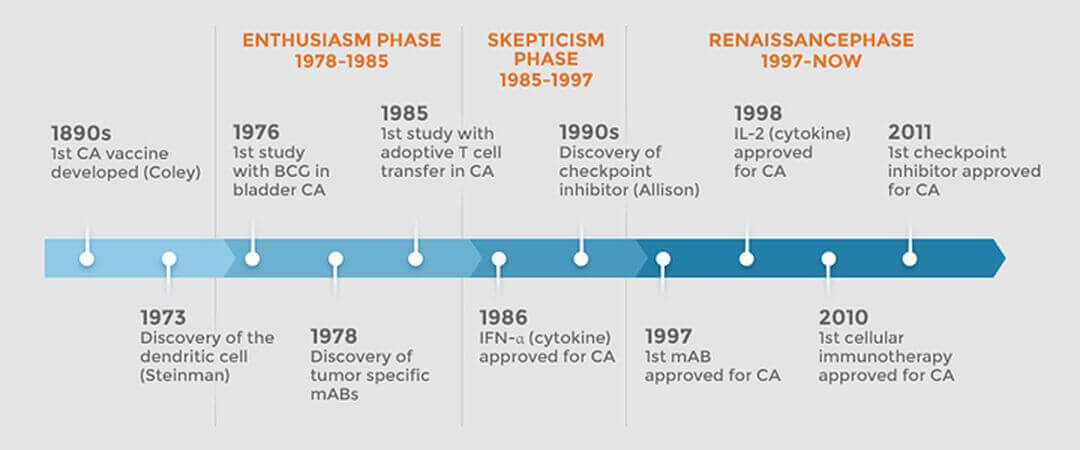
Immunotherapy has been part of the medical lexicon since the 1890s and has entered a renaissance phase. Fifteen FDA-approved immunotherapy agents have been approved since 1986. Currently approved immunotherapy agents target more than 10 different cancer types.
There are more than 600 ongoing immunotherapy clinical trials for cancers such as breast, colon, head and neck, and kidney.
“The immunotherapy concept is simple: unleash the body’s immune system to attack cancer,” said Dr. Julie Vose, president of the American Society of Clinical Oncology. “It has proven extremely difficult, however, to develop treatments that deliver real, consistent results. Decades of bold ideas, dedication, and financial investment in research have been required to prove immunotherapy’s worth as a treatment for people with an array of different cancers.”
She announced no recent advance has been more transformative than the rise of immunotherapy, particularly during the past year, making immunotherapy the ASCO’s Advance of the Year for 2016.
Cancer remains a leading cause of death in the United States, claiming approximately 600,000 lives in 2015. [1] Globally, seven of every 10 cancer deaths occur in Africa, Asia, and Central and South America. By 2030, these cancer deaths could increase by as much as 80 percent, according to World Health Organization estimates.
More research and education needed
Cancer cells thrive because they are able to hide from the immune system. Immunotherapies can mark cancer cells so the immune system can find and destroy them. Other immunotherapies boost your immune system to work better against cancer.
“For the longest time, people did not believe this was possible,” said Lawrence Fong, MD, associate professor of medicine at the University of California-San Francisco and one of the university’s lead investigators in the expanding use of immunotherapy. [2]
“Now we can treat cancer by treating the patient instead of the disease,” Dr. Fong said. “That’s the biggest change. We can treat cancer without delivering chemotherapy or radiation to kill the cancer or performing surgery to get rid of the tumor.”

“Lack of knowledge about herbs and supplements, and awareness of that lack of knowledge is probably one of the reasons why oncologists don't initiate the discussion.”
Dr. Richard Lee
MD Anderson Cancer Center
A study published in the Journal of Clinical Oncology noted that fewer than half of oncologists bring up the subject of herbs or supplements with their patients. Many doctors cited their own lack of information as a major reason why they skip that conversation. [3]
“Lack of knowledge about herbs and supplements and awareness of that lack of knowledge is probably one of the reasons why oncologists don't initiate the discussion,” said the study's author, Dr. Richard Lee, medical director of the Integrative Medicine Program at the University of Texas MD Anderson Cancer Center.
“It's really about getting more research out there, and more education, so oncologists can feel comfortable having these conversations,” Dr. Lee said.
A healthy immune system is the most important thing in the fight against cancer. “Cancer first and foremost is a problem with the immune system. You cannot have cancer if you have an intact immune system,” Dr. Rashid Buttar said.
Not only is a weak immune system a major reason patients have cancer — but cancer itself can further weaken the immune system.
An amplified immune system response
The immune system contains many different types of cells, however, only a handful of these white blood cells actually kill cancer cells. It should be the intent of a person with cancer to focus on treatments that quickly increase the count of the cancer-killing white blood cells.
Beta 1,3-D Glucan works by activating the macrophages, or immune cells, which trap and engulf foreign substances. These activated cells start a cascade of events that cause the entire system to be alerted and mobilized in an entirely naturally activated sequence. This amplified immune system response helps speed up the recovery of damaged tissue, helps other substances like antibiotics, antifungals, and antiparasitics to work better, and helps the macrophages recognize and destroy mutated cells.
Beta glucan is an immunomodulator which helps make your immune system smarter. In short: Beta glucans help regulate the immune system, making it more efficient. Beta glucan can help raise your immune system’s response so your body can naturally fight off and kill cancer. Beta glucan stimulates white blood cells (lymphocytes) that bind to tumors or viruses and release chemicals to destroy it.
Beta glucan has been approved in Japan, Australia, South Korea, and Taiwan as an immunoadjuvant therapy for cancer. There have been many studies showing the product can protect against infections, lower your cholesterol, lower blood sugar, reduce stress, increase your antibody production, heal wounds, help radiation burns, overcome mercury-induced immunosuppression (like Thimerosal, used as a preservative in vaccines), help with diabetes, and even naturally prevent metastasisThe spread of cancer cells from the place where they first formed to another part of the body. In metastasis, cancer cells break away from the original (primary) tumor, travel through the blood or lymph system, and form a new tumor in other organs or tissues of the body. The new, metastatic tumor is the same type of cancer as the primary tumor. For example, if breast cancer spreads to the lung, the cancer cells in the lung are breast cancer cells, not lung cancer cells. (or the spreading of your cancer).
Healthy living for immunotherapy
As Laurie McGinley reported in The Washington Post, researchers caution that they have a long way to go in fully understanding the therapy and transforming it into a viable treatment for a majority of patients. “This period for immunotherapy is comparable to the 1960s for chemotherapy when we were just beginning to use it,” said Roy Jensen, director of the University of Kansas Cancer Center. “There is so much to do and to figure out. We’re just at the start of this.” [4]
Harvard Medical School notes the first line of defense is a healthy lifestyle. Adhering to good-health guidelines is the single best step to take toward keeping your immune system strong. Every part of your body, including your immune system, functions better when protected from environmental assaults and bolstered by healthy-living strategies:
- Don't smoke.
- Eat a diet high in fruits, vegetables, and whole grains, and low in saturated fatA type of fat with certain chemical properties that is usually solid at room temperature. Most saturated fats come from animal food products, but some plant oils, such as palm and coconut oil, also contain high levels. Eating saturated fat increases the level of cholesterol in the blood and the risk of heart disease..
- Exercise regularly.
- Maintain a healthy weight.
- Control your blood pressure.
- If you drink alcohol, drink only in moderation.
- Get adequate sleep.
- Take steps to avoid infection, such as washing your hands frequently and cooking meats thoroughly.
- Get regular medical screening tests for people in your age group and risk category.
The immune system relies on the stomach. A healthy immune system needs good, regular nourishment. Scientists have long recognized that people who live in poverty and are malnourished are more vulnerable to infectious diseases.
There is some evidence that various micronutrient deficiencies — zinc, selenium, iron, copper, folic acid, and Vitamins A, B6, C, and E — alter immune responses in animals, as measured in the test tube. However, the impact of these immune system changes on the health of animals is less clear, and the effect of similar deficiencies on the human immune response has yet to be assessed. But the research at this stage is promising, at least for some of the micronutrients.
If your diet is not providing all necessary micronutrient needs — maybe you don't like vegetables or you choose white bread over whole grains — taking a daily multivitamin and mineral supplementA product, generally taken orally, that contains one or more ingredients (such as vitamins or amino acids) that are intended to supplement one's diet and are not considered food. brings health benefits of many types, beyond any possibly beneficial effects on the immune system. [5]
Boost your immune system with probiotics
Probiotics are naturally found in your body. You can also find them in some foods and supplements — in everything from yogurt to chocolate. Probiotics are generally from two groups:
Lactobacillus — The most common probiotic, this is found in yogurt and other fermented foods. Different strains can help with diarrhea and may help with people who can’t digest lactose, the sugar in milk.
Bifidobacterium — This also is found in some dairy products. It may help ease the symptoms of irritable bowel syndrome (IBS) and some other conditions.
Probiotics help move food through your gut. Examples of probiotic foods you should look to consume include: fermented vegetables (sauerkraut, kimchi), probiotic yogurt (from goat or sheep milk that is grass-fed and organic), fermented dairy products (kefir), probiotic beverages (apple cider vinegar, coconut kefir, kvass), kombucha, natto, raw cheese (goat’s milk, sheep’s milk, A2 cow’s soft cheeses).
Orthodox medicine immunotherapies
Conventional immunotherapies fall into four general categories:
- Checkpoint Inhibitors — disrupt signals that allow cancer cells to hide from an immune attack;
- Cytokines — protein molecules that help regulate and direct the immune system;
- Cancer vaccines — used to treat and prevent cancer by targeting the immune system;
- Monoclonal Antibodies (mAbs) — elicit a direct or indirect immune response that leads to cell death.

“The immunotherapy concept is simple: unleash the body’s immune system to attack cancer.”
Dr. Julie Vose
President, ASCO
However, the immune system has a blind spot; the ability to attack itself leads to autoimmune diseases. For protection, the immune system screens out its own tissue. Cancer cells are not recognized as invaders because they are the body’s own cells that have mutated. The immune system doesn’t recognize this distinction.
One way cancerous cells stay hidden is by sending signals to the PD-1 CTLA-4 receptors at certain checkpoints on immune cells. Those signals trick the body into thinking the cancer cells are normal.
Checkpoint inhibitors allow cancer cells to be exposed and trigger an immune system response. Cytokines and cancer vaccines also generate an immune response by helping the body recognize cancer cells.
Two non-specific immunotherapies are:
Interferons — help the immune system fight cancer and may slow the growth of cancer cells. An interferon made in a laboratory, called interferon alpha (Roferon-A [2a], Intron A [2b], Alferon [2a]), is the most common interferon used in cancer treatment. Side effects of interferon treatment may include flu-like symptoms, an increased risk of infection, rashes, and thinning hair.
Interleukins — Interleukins help the immune system produce cells that destroy cancer. An interleukin made in a laboratory, called interleukin-2, IL-2, or aldesleukin (Proleukin), is used to treat kidney cancer and skin cancer, including melanoma. Common side effects of IL-2 treatment include weight gain and low blood pressure, which can be treated with other medications. Some people may also experience flu-like symptoms.
The Food and Drug Administration has approved four checkpoint inhibitors — manufactured drugs that unleash an immune system attack on cancer cells:
- Yervoy (ipilimumab) produced by Bristol-Myers Squibb
- Keytruda (pembrolizumab) produced by Merck
- Opdivo (nivolumab) produced by Bristol-Myers Squibb
- Tecentriq (atezolizumab) produced by Genentech (Roche Pharmaceutical)
Clinical trials are under way to treat a variety of cancers with vaccines:
Tumor cell vaccines — made from cancer cells that have been removed from the patient. The cancer cells are altered in the lab (made to be more likely to be attacked by the immune system) and injected back into the patient. The immune system response should be to attack the cells and kill them.
Antigen vaccines — boost the immune system by using only select antigen(s). The antigens are usually proteins or pieces of proteins (peptides). These vaccines can be specific for a certain type of cancer, but they are not made for a specific patient.
Dendritic cell vaccines — focus on cells in the immune system that recognize cancerous cells. They break down cancer cells into smaller pieces (including antigens) and then hold out these antigens so T cells can see them. The T cells then start an immune reaction against any cells in the body that contain these antigens.
Vector-based vaccines — special viruses, bacteria, yeast cells, or other structures used to get antigens into the body. The vectors are often germs that have been altered to make sure they can no longer cause disease. Vectors can deliver more than one cancer antigen at a time, which might make the body’s immune system more likely to mount a response. Viruses and bacteria also may trigger their own immune responses, which could help make the overall response even stronger.
Among the cancers for which vaccines are being studied:
- Brain tumors (especially glioblastoma)
- Breast cancer
- Cervical cancer
- Colorectal cancer
- Kidney cancer
- Lung cancer
- Lymphoma
- Melanoma
- Pancreas cancer
- Prostate cancer
Monoclonal antibodies used in cancer treatment: [6]
Naked monoclonal antibodies — no drug or radioactive material is attached and these are the most common type of mAbs used to treat cancer. The antibodies boost the immune response against cancer cells by attaching to them and acting as a marker for the body’s immune system to destroy them or blocking antigens on cancer cells (or other nearby cells) that help cancer cells grow or spread.
Conjugated monoclonal antibodies — joined to a chemotherapy drug (Chemolabeled antibodies) or to a radioactive particle (Radiolabeled antibodies). The mAb is used as a homing device to take one of these substances directly to the cancer cells.
Bispecific monoclonal antibodies — made up of parts of two different mAbs, meaning they can attach to two different proteins at the same time. One part attaches to the CD19 protein and another part attaches to CD3, a protein found on T cells. By binding to both proteins, this drug brings the cancer cells and immune cells together, which is thought to cause the immune system to attack the cancer cells.
Orthodox medicine and side effects
According to the IMS Institute for Healthcare's Global Outlook for Medicines Through 2018 report, there are 374 experimental cancer drugs in mid-stage trials.
There a huge medical need from patients, for whom many new treatments extend lives by years, rather than months. And the financial reward for drugmakers is huge. The drugs have annual costs of $150,000 or more, and a slate of personalized treatments are expected to carry even higher price tags.
Companies are pushing related immune-oncology drugs that will be used in combination with one another. While their drugs have only shrunk tumors in about 30 percent of the population, combinations may help broaden their use — but safety studies are not done on these combinations and none of these drugs offer an outright cure.
FDA-approved checkpoint inhibitors and their published side effects:
Yervoy is a drug marketed as an adjuvant treatment for Stage III melanoma (to help prevent melanoma from coming back after surgery to remove the tumor and lymph nodes that contain cancer) and for metastatic melanoma (that has spread or cannot be removed by surgery). Yervoy can cause serious side effects in many parts of your body which can lead to death. These serious side effects may include:
- Intestinal problems (colitis) that can cause tears or holes (perforation) in the intestines;
- Liver problems (hepatitis) that can lead to liver failure;
- Skin problems that can lead to a severe skin reaction;
- Nerve problems that can lead to paralysis;
- Hormone gland problems (especially the pituitary, adrenal, and thyroid glands);
- Eye problems.
Keytruda is a drug that may treat melanoma or lung cancer or head and neck cancer by working with the immune system. Keytruda can cause the immune system to attack normal organs and tissues in many areas of the body and can affect the way they work. These problems can sometimes become serious or life-threatening and can lead to death.
- Lung problems (pneumonitis);
- Intestinal problems (colitis) that can lead to tears or holes in your intestine;
- Liver problems (hepatitis);
- Hormone gland problems (especially the thyroid, pituitary, adrenal glands, and pancreas);
- Kidney problems, including nephritis and kidney failure;
- Problems in other organs;
- Infusion (IV) reactions, that can sometimes be severe and life-threatening;
- If you are pregnant or plan to become pregnant, tell your doctor. Keytruda can harm your unborn baby.
Opdivo is a drug for previously treated metastatic non-small cell lung cancer; for patients with metastatic melanoma across BRAF status; for advanced renal cell carcinoma patients who received prior anti-angiogenic therapy; and for previously treated patients with advanced classical Hodgkin lymphoma.
- Lung problems (pneumonitis);
- Intestinal problems (colitis) that can lead to tears or holes in your intestine;
- Liver problems (hepatitis);
- Hormone gland problems (especially the thyroid, pituitary, adrenal glands, and pancreas);
- Kidney problems, including nephritis and kidney failure;
- Skin problems;
- Inflammation of the brain (encephalitis);
- Problems in other organs.;
- Severe infusion reactions;
- Complications of stem cell transplant that uses donor stem cells (allogeneic) after treatment with Opdivo;
- Tell your healthcare provider if you are pregnant or plan to become pregnant.
Tecentriq is a drug for the treatment of patients with locally advanced or metastatic urothelial carcinoma who have disease progression during or following platinum-containing chemotherapy, or have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy. It also can have serious side effects:
- Immune-related pneumonitis;
- Immune-related hepatitis;
- Immune-related colitis;
- Immune-related endocrinopathies;
- Other immune-related adverse reactions;
- Infection;
- Infusion-related reactions;
- Embryo-fetal toxicity.
Foods to boost the immune system
Building and maintaining a strong, healthy immune system takes time, and food has a significant role in immune system health. The key to a healthy diet is the correct mix of vitamins and minerals. Beyond that, the immune system also needs a balance with adequate sleep and exercise.
Vitamin A — Choose foods that are high in carotenoids — carrots, sweet potatoes, pumpkin, cantaloupe, and squash. The body turns these carotenoids into Vitamin A. These foods also have an antioxidant effect to help strengthen the immune system.
Vitamin B6 — Foods high in Vitamin B6 include bananas, lean chicken breast, cold-water fish (tuna), baked potatoes, and chickpeas (hummus). Vitamin B6 is part of nearly 200 biochemical reactions in the body and is critical in how the immune system functions.
Vitamin C — It's not just in OJ, you know. While many get their Vitamin C from citrus juices (oranges, grapefruits, guava, and strawberries), leafy green vegetables also are a great source. Up your daily intake with bell peppers, broccoli, Brussels sprouts, kale, and spinach.
Vitamin D — Fatty fish (mackerel, salmon, sardines, and tuna) are high in Vitamin D, as are cereals, milk, and orange juice. However, if you have a Vitamin D deficiency a vitamin supplement may be your best option and should be discussed with a doctor.
Vitamin E –Almonds, broccoli, hazelnuts, spinach, and sunflower seeds are high in Vitamin E, and can be an antioxidant to help fight infection. Its immune function role has been shown in vitro studies of cells, cell signaling, regulation of gene expression, and other metabolic processes.
Folate — Beans and peas as well as leafy green vegetables have natural folate. Folic acid — the synthetic form of folate — is in supplements and fortified foods like enriched bread, pasta, rice, and other 100 percent whole-grain products.
Iron — This nutrient is an essential component of hemoglobin, an erythrocyte protein that transfers oxygen from the lungs to the tissues. The body can more easily absorb “heme iron” abundant in lean poultry (chicken and turkey) plus seafood. Other forms of iron are in beans, broccoli, and kale.
Selenium — Skeletal muscle is the major site of selenium storage and has a powerful effect on the immune system. Selenium is in barley, brazil nuts, broccoli, garlic, sardines, and tuna, among other foods. Selenium has the potential to slow the body’s overactive responses to certain aggressive forms of cancer.
Zinc — This essential trace element found in cells helps slow down the immune response and control inflammation in the body. Chickpeas, crab, baked beans, lean meats and poultry, oysters, and yogurt are good sources of zinc.
Don't forget sleep and exercise
Supporting the role of chronic sleep loss in the long-term development of pathologies is accumulating evidence that sleep itself has a substantive role for the functioning of the immune system, whereas sleep loss is a risk factor for impaired immune function. [7]
Many immune parameters show systematic fluctuations over the 24-hour day in human blood. Circulating naive T cells and production of proinflammatory cytokines, like interleukin-12 (IL-12), peak during nighttime, whereas cytotoxic effector leukocytes and production of the anti-inflammatory cytokine IL-10 peak during daytime. These temporal changes originate from a combined influence of the circadian system and sleep. Both brain functions act synergistically and share neuroendocrine effector mechanisms to convey control over immune functions. [8]
Exercise has been shown to increase the production of macrophages, important cells of the immune system that are formed in response to an infection or accumulating damaged or dead cells. Also when we exercise, the increase in body temperature may inhibit the growth of bacteria. Some researchers believe regular exercise helps rid the lungs of bacteria and viruses that cause upper respiratory tract infections.
The American College of Sports Medicine report on The Recommended Quantity and Quality of Exercise for Cardiorespiratory Fitness in Healthy Adults recommends any activity that uses large muscle groups, which can be maintained continuously, and is rhythmical and aerobic in nature, e.g., walking, hiking, running-jogging, cycling-bicycling, cross-country skiing, aerobic dance / group exercise, rope skipping, rowing, stair climbing, swimming, skating, and various endurance game activities or some combination thereof.
References
1. Robert C, Schachter J, Long GV, et al; KEYNOTE-006 investigators: Pembrolizumab versus ipilimumab in advanced melanoma. N Engl J Med 372:2521-2532, 2015
2. Killing Cancer Through the Immune System by Michael Howerton | Feb. 4, 2014
3. National Survey of US Oncologists’ Knowledge, Attitudes, and Practice Patterns Regarding Herb and Supplement Use by Patients with Cancer by Dr. Richard T. Lee | November 2014
4. The list of cancers that can be treated by immunotherapy keeps growing by Laurie McGinley | April 19, 2016
5. How to boost your immune system | Harvard Medical School | June 15, 2016
6. Monoclonal antibodies to treat cancer | American Cancer Society
7. Ackermann K; Revell VL; Lao O; Rombouts EJ; Skene DJ; Kayser M. Diurnal rhythms in blood cell populations and the effect of acute sleep deprivation in healthy young men. SLEEP 2012;35(7):933-940.
8. Lange T, Dimitrov S, Born J. Effects of sleep and circadian rhythm on the human immune system. Ann N Y Acad Sci. 2010;1193:48–59.
